Growing functional human organs outside the body is a long-awaited “holy grail” of organ transplant medicine that remains out of reach. New research from the Harvard Wyss Institute for Biologically Inspired Engineering and the John A. Paulson School of Engineering and Applied Science (SEAS) brings this goal a big step closer.
Published in the journal Advanced Materials, the study describes the new technique, called “coaxial SWIFT” (co-SWIFT). This method builds on an earlier technique called “sacrificial writing in functional tissue” (SWIFT), which creates hollow channels within a living cell matrix.
“In prior work, we developed a new 3D bioprinting method, known as ‘sacrificial writing in functional tissue’ (SWIFT), for patterning hollow channels within a living cellular matrix. Here, building on this method, we introduce coaxial SWIFT (co-SWIFT) that recapitulates the multilayer architecture found in native blood vessels, making it easier to form an interconnected endothelium and more robust to withstand the internal pressure of blood flow,” said first author Paul Stankey, a graduate student at SEAS in the lab of co-senior author and Wyss Core Faculty member Jennifer Lewis, Sc.D.
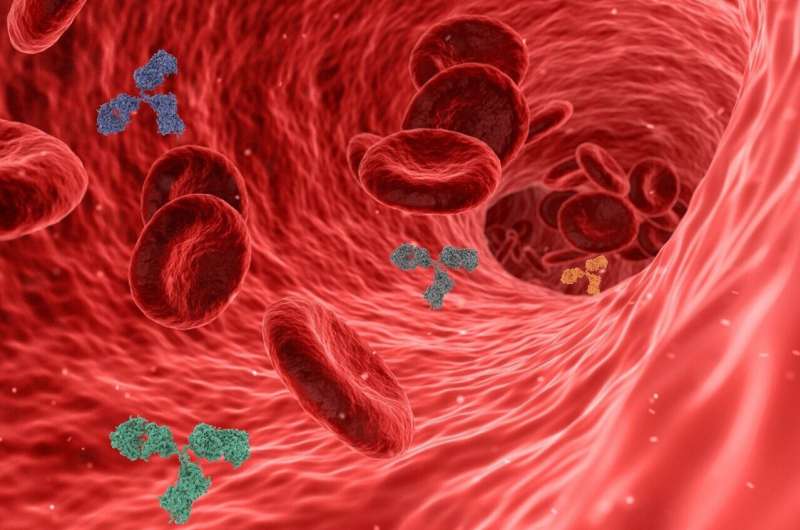
The key to the innovation lies in a special nozzle with two independently controllable fluid channels for the printing materials: a collagen-based shell ink and a gelatine-based core ink. This nozzle makes it possible to completely penetrate the previously printed vessels and create branched networks that ensure sufficient oxygen supply to the tissue. The size of the vessels can be varied by adjusting the printing speed or the flow rates of the inks.
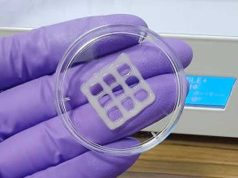
To verify the method, the team printed their multilayered vessels first in a transparent, granular hydrogel matrix and then in a porous, collagen-based matrix called uPOROS. After printing, the matrix was heated, which cross-linked the collagen and melted the gelatin core ink, allowing for easy removal and resulting in an open, permeable vasculature.
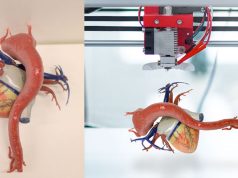
“We were able to successfully 3D-print a model of the vasculature of the left coronary artery based on data from a real patient, which demonstrates the potential utility of co-SWIFT for creating patient-specific, vascularized human organs,” said Lewis, who is also the Hansjörg Wyss Professor of Biologically Inspired Engineering at SEAS.
In a further step, the team printed vessels with a coating ink enriched with smooth muscle cells (SMCs) and then perfused them with endothelial cells (ECs). After one week of perfusion, the cells functioned as vessel walls, with the permeability of the vessels decreasing threefold.
Finally, the researchers tested their method in living human tissue. They created hundreds of thousands of tiny, beating heart cell blocks and printed a biomimetic vascular network on them. After removing the nuclear ink and perfusing with ECs, the heart tissue blocks began to beat synchronously after five days and responded to common cardiac drugs.
The researchers also printed a model of a real patient’s left coronary artery, demonstrating the technique’s potential for personalized medicine.
“To say that engineering functional living human tissues in the lab is difficult is an understatement. I’m proud of the determination and creativity this team showed in proving that they could indeed build better blood vessels within living, beating human cardiac tissues. I look forward to their continued success in their quest to one day implant lab-grown tissue into patients,” said Wyss Founding Director Donald Ingber, M.D., Ph.D.
Subscribe to our Newsletter
3DPresso is a weekly newsletter that links to the most exciting global stories from the 3D printing and additive manufacturing industry.